While sleeping baby in their own sleeping environment cot is always the safest option, this is not always possible – especially if you have twins.

Red Nose recommends six key steps to help reduce the risk of sudden infant death and sleeping accidents:
1. Always place baby on their back to sleep, not on the tummy or side
2. Keep baby’s face and head uncovered
3. Keep baby smoke free before birth and after
4. Safe sleeping environment night and day
5. Sleep baby in their own safe cot in the same room as an adult care-giver for the first six to twelve months
6. Breastfeed baby
The term Sudden Unexpected Death in Infancy (SUDI) is now used as this term refers to all cases of sudden and unexpected death in infancy and includes deaths from Sudden Infant Death Syndrome (SIDS) and fatal sleeping accidents. Safe sleeping recommendations target known risk factors associated with SUDI. Where studies specifically define the population as SIDS, this specific term will be used to describe the study findings.
- Occasionally twins share the same cot in hospital in the first few weeks of life while in the care of health professionals and monitored
- Research has shown that the safest way to sleep twins in the home is in their own safe sleeping place (cot, portable cot) in the parents’ room for the first 6-12 months
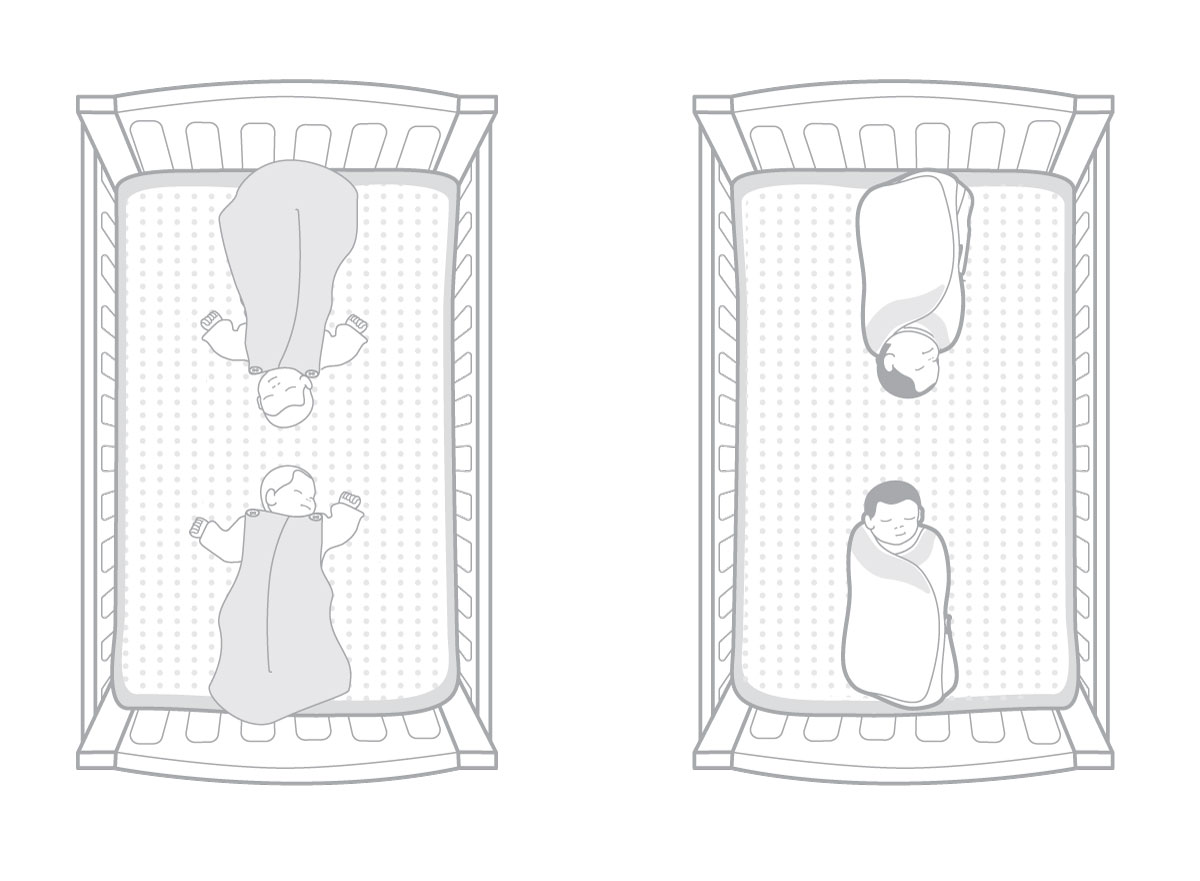
- Sometimes twin babies are in temporary situations, such as while visiting or travelling, when separate cots are not possible. If twins must share the same sleep space, a cot is the most suitable, do not use bedding (such as sheets and blankets) and place them at opposite ends of the cot. An infant sleeping bag used for each baby may be useful in this situation.
- When the babies have reached the age where they can move freely around the cot, they must be placed in separate cots.
- Babies should not co-bed with any other children.
Premature and low birth weight babies are at increased risk of SUDI 1-3. Blair et al (2006) concluded that ‘the combined effects of SUDI risk factors in the sleeping environment and being pre-term or low birth weight generate high risks for these babies. Their longer postnatal stay allows an opportunity to target parents and staff with risk reduction messages.1
Definition
Co-bedding means placing siblings from multiple births on the same sleep space (cot or incubator) 4
Incidence of multiple births
Multiple births have increased in recent years as a result of delayed pregnancy and use of fertility therapy and there are increased numbers of premature and multiple-birth neonates cared for in Neonatal Intensive Care Units (NICUs) 5.
Below are the Red Nose recommendations for sleeping twins safely. For higher order multiple births (triplets, quadruplets, quintuplets), please refer to your health professional for advice on providing a safe sleep environment for each baby.
Co bedding in the hospital setting
Co-bedding of twins was introduced in neonatal units predominately in the US from the 1990s. In utero, twins interact with each other through activities like touching or holding termed “co-regulation”. Co-bedding aimed to continue this fetal co-regulation and potentially promote growth and neurodevelopment 6,7. Other proposed advantages of co-bedding include heat conservation, apnea reduction, improved bonding between infants, improved parental and staff satisfaction 6, and saving of cot space.
However, concerns regarding co-bedding include risk of infection, possible medication error, difficulties involving the routine care of individual infants, less reliable incubator temperature control, mutual disturbance leading to reduced sleep quality, and possible physical injury 7.
A recent Cochrane Review 8 included six mostly small studies with some limitations in their methods. All studies were conducted in the neonatal nursery of a major tertiary hospital and enrolled preterm infants of average postmenstrual age of 29 weeks. Overall, the review reported no differences between the co-bedded group and the group receiving care separately in terms of weight gain, episodes of major disturbances in their breathing, heart rate or oxygenation level (apnea, bradycardia, or desaturation episodes), length of hospital stay, and occurrence of infection. Conflicting results were noted in the two included studies that assessed infants’ pain response after heel prick.
Current research into the co-bedding of twins does not provide sufficient evidence to guide policy and guidelines for or against the practice in NICU 8,9. More research is required. Health professionals in NICUs or Special Care Nurseries (SCNs) must weigh up the risks and benefits for each baby. A significant consideration in this risk/benefit assessment must be the care and safety of babies when they are discharged home as many parents will continue infant care practices modelled by hospital staff 4 .
Prior to discharge from hospital
Nursing staff and midwives should use the back sleeping position for all babies prior to discharge to establish a safe sleeping model for parents to follow when their baby is discharged.
When the babies are ready for discharge, staff should ensure that the parents know how to reduce the risk of SUDI and fatal sleep accidents. It should not be assumed that parents have this information already as they may have missed other opportunities to learn about safe sleeping environments for babies.
Sleeping twins safely at home
Although surveys demonstrate that co-bedding twins at home is common (> 50%) 10,11, current evidence shows that the safest way to sleep twins at home is to place them in their own cot and follow the Red Nose safe sleeping guidelines. These guidelines aim to reduce the risk of SUDI, including SIDS and fatal sleep accidents. The American Academy of Pediatrics also advises separate sleep surfaces and to avoid co-bedding for twins (and higher order multiples) in both hospital and at home 12.
Co-bedding twins would be dangerous if one part of the body of one twin were able to accidentally cover the face of the other causing an interference with breathing. A small observational study of 10 twin pairs sleeping in various side by side and head to head configurations showed that twins sleeping side by side occasionally impinged on, although did not obstruct, the airway of the other twin 13 .
Sleeping twins safely when separate cots are not available
Sometimes parents and carers of twins may need to sleep twins in the same cot temporarily, for example when travelling or visiting, if there is insufficient space for two cots in the room. In these circumstances, ways to minimise the risks for twin babies sharing the same cot include:
- Place the babies head to head, at opposite ends of the cot (see diagrams below)
- Never place the baby in the cot with any other children
- Do not use bedding. Safe alternatives to bedding include:
- Wrap the babies separately according to Red Nose guidelines (from birth until showing signs of being able to roll over)
- Sleep the babies in separate safe infant sleeping bags (for babies weighing 3.2kg and over)
When the babies are able to move freely around the cot, place them to sleep in separate cots.
For more information on the sleeping of twins at home visit the Red Nose website at rednose.org.au.
In Australia, between 1990 and 2015 approximately 5,000 babies died suddenly and unexpectedly. Baby deaths attributed to SUDI have fallen by 85% and it is estimated that 9,967 infant lives have been saved as a result of the infant safe sleeping campaigns.
The Safe Sleeping program is based on strong scientific evidence, has been developed in consultation with major health authorities, SUDI researchers and paediatric experts in Australia and overseas, and meets the National Health & Medical Research Council rules for strong evidence.
For further information visit the Red Nose website at rednose.org.au or phone us on 1300 998 698.
Suggested citation:
Red Nose. National Scientific Advisory Group (2017). Information Statement: Co-bedding twins. Melbourne, Red Nose. This information statement was first posted in October, 2010. Most recent revision March 2017.
Last modified: 7/1/21
